Clinical Decision Support Systems
Hello and welcome, happy readers! I hope you are well and in good health in these difficult times.
Today I would like to talk to you about clinical decision support systems- early implementations, the existing types, and state of the art techniques.
Clinical decision support systems (CDSS) are computer-based programs that support clinicians in their decision-making process by providing information extracted from patient data. One of the earliest implementations of a CDSS is the MYCIN system developed by Edward Shortliffe in the early 1970s. If you are well versed in clinical lingo, the name may already reveal to you what the goal of MYCIN was: the recommendation of antibiotics to patients with bacterial infections (antibiotics often carry the suffix “-mycin”).
MYCIN was designed with several constraints in mind. To motivate clinicians to participate in the project, a task had to be chosen that would be of the clinicians’ interest. Previous research indicated that antibiotics were often administered inefficiently, making the topic a valuable target for decision support. Given the complexity and continuous evolution of the medical field, the system needed to manage a large, constantly changing body of information, as well as possess the ability to communicate with the user effectively. Results that were computed by the system needed to be explained to the user- the systems aim was to support physicians rather than replace them. After all, engineers will gladly assist clinicians, but we will not take responsibility for patient outcomes. 😉
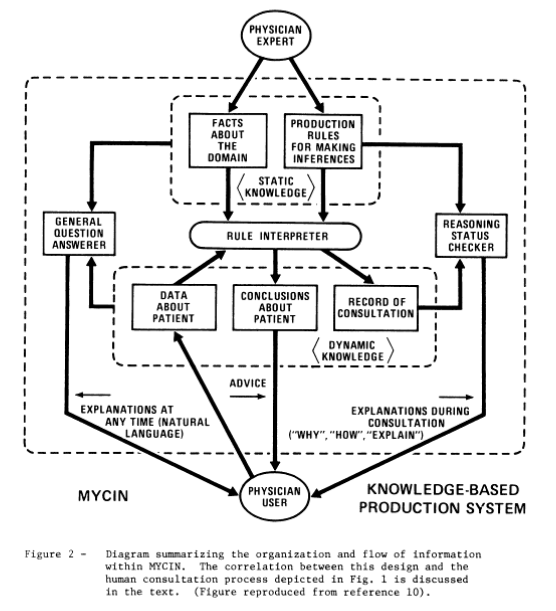
Due to the design requirements, MYCIN needed several interacting components each responsible for a subtask. At MYCINs core was the knowledge base, and a patient database, which both fed a group of subsystems: the consultation system, the explanation system, the question answering system, and the knowledge acquisition system.
– The consultation system gave advice to the clinician regarding the recommended therapy, based on inferences performed on the knowledge database and the patient database.
– The explanation system gave information regarding the reasoning behind recommended therapy and the knowledge base.
– The question answering system allowed the clinician to obtain information regarding the knowledge database, and the specific consultation.
– The knowledge acquisition system allowed the physician to extend MYCINs existing knowledge database with new information.
MYCIN employed a paradigm of certainty factors to assess the certainty of diagnoses and recommendations that it suggested. Possible diagnoses were first accumulated and then filtered by a predefined threshold and probabilities of the diagnoses were computed. To allow for efficient computation and prevent excessive input requirements (endless questions to the clinician), MYCIN started by asking the physician questions which could result in diagnoses with a high certainty.
While the MYCIN system was developed for a specific task, the general idea of the architecture was that it could be applied to other domains. This could only happen under certain constraints: The domain of application must be developed far enough to have a certain degree of formalization. Basic processes must be understood to create rules and certainty factors. Additionally, it is important that there is a limited connection between different concepts, and that the knowledge base is created by domain experts who speak the same language as the final users. Different concepts needed to be understood by end-users and the used terminology had to be non-ambiguous.
Due to transparency and explanation being among the most important factors for and CDSS, MYCIN was designed to display the rules that it uses to obtain its conclusions. Post consultation, the system can remember the rules which it invoked and based on which data these rules were invoked. MYCIN was able to use its knowledge base to answer questions that are asked by clinicians. Because the usefulness of displaying certain rules- such as definitions- is limited, the authors implemented a metric to measure the usefulness of displaying rules depending on their resulting certainty factor. Even though there is no formal justification for this approach, it appears that the metric allows the system to prioritize displaying non-trivial information and is very useful in practice.
You may now wonder how popular MYCIN was during its time, and how successful its deployment was. While a blind study showed MYCIN to have a performance similar or better than leading physicians at Stanfords medical center [2], it was never fully deployed. MYCIN came before the personal computer was developed, and therefore could not be used efficiently by clinicians. It does, however, remain one of the milestones in the development of CDSS and explainable artificial intelligence systems.
Modern CDSS can generally be divided into three different categories, differing by the techniques that they used to perform inferences: knowledge based (such as MYCIN), non-knowledge based, and hybrid CDSS.
– Knowledge based CDSS perform inference on a knowledge base. Knowledge bases may come in different forms, such as production rules, ontologies, etc. The key thing to remember is that the terminology used must be shared across all users. The construction of such knowledge bases is usually a cooperation between domain experts (clinicians), and knowledge engineers. Such systems use a deductive reasoning process (“The patient will benefit from treatment X, because the patient has property Y, which indicates Z.”) The explicit hard coding of symbolic concepts (diseases, clinical findings, patient parameters) in conjunction with explainable rules allows for a high degree of explainability.
– Non-knowledge based CDSS use mathematical models, such as machine learning algorithms, which are first trained on large databases, and then deployed on the data obtained from individual patients. The reasoning process in inductive (“The patient will benefit from treatment X, because other patients with similar properties benefitted from treatment X.”). While such systems often show significantly better performance, they lack explainability.
– Hybrid systems strive to provide the best of both worlds. They integrate knowledge bases for explainability and use machine learning to extract information from patient data. The extracted information may be mapped to symbolic elements, for which explainable rules exist. Data is therefore processed with high performance systems, but inference is co-performed using a fully explainable system. Naturally, training machine learning models to map to symbolic elements requires training data that contains labels for the symbols that we want to extract, which requires an expensive and time-consuming labelling process.
Un abrazo,
Alex 🙂
[1] Shortliffe EH. Mycin: A Knowledge-Based Computer Program Applied to Infectious Diseases. Proc Annu Symp Comput Appl Med Care. 1977;66-69.
[2] Harmon, P., & King, D. (1986). Expert systems: Artificial intelligence in business. In Expert systems: Artificial intelligence in business (pp. 20-21). Taipei: Kai Fa Book.
