Duel of Fates -
or "Am I an atrial cell yet?"
Heart cell specification and differentiation
The human body is made up of a lot of cells and most of them are very specialized: letting them bear loads, absorb nutrients, secrete hormones or process blog posts about specialized cells. The heart is no different in this aspect, although its purpose seems singular (pumping blood), a whole team of cells is needed to achieve this, including cells creating blood vessels to supply the organ, cells giving electrical impulses to induce pumping and of course actual muscle cells doing the heavy lifting (or more appropriately pulling). The heart however has even differing muscles cells for this job, with the two prominent types being ventricular cells (those contracting the ventricle) and atrial cells (contracting the atrium) and there are some specifics making them not so similar after all. In case you are really interested in how they differ, here is a link to a comprehensive review on the topic (identities of atrial cardiomyocytes).
But in short, some aspects are: atrial muscle cells beat faster, have almost no T-Tubules (an integral structural component of ventricular cells), express some different ion channels and have shorter action potential durations with no plateaus. They are a bit the faster ticking little brother of ventricular cells (please don’t cite this). And to study a disease that effects the atrium (like atrial fibrillation) we need exactly these cells.
Contracting cells – …but could you tell what kind they are?
The human body gets atrial cells through self organization. During embryo development cells continuously secrete factors to their surroundings. Because of the differing positions of each cell (for example at the edge of the embryonic body or its core) a “gradient”” or differing concentration of these factors in the different sections of the embryo is created (for example more of a factor at the center of a cell group). As cells experience distinct signals due to these deviating concentrations, the result is them differentiating into various cell types, like our heart muscle cells.
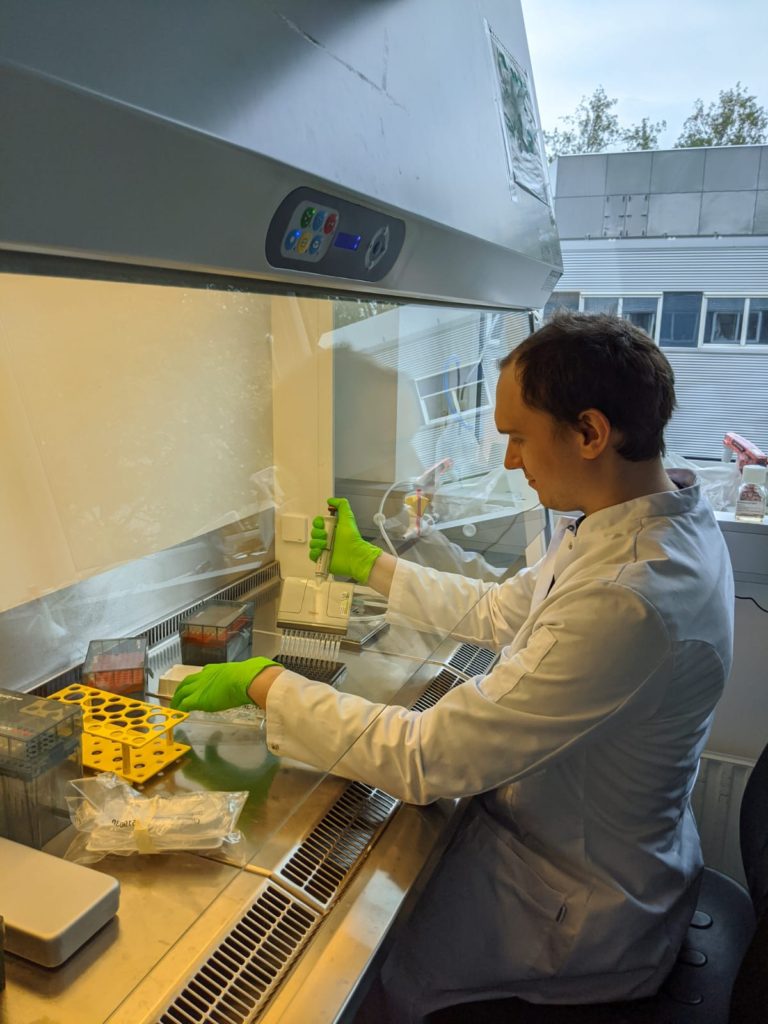
Using these native atrial heart muscle cells of a patient in the lab to study disease is however difficult, as their extraction could be harmful and they cannot be maintained in the lab for a long time. Therefore utilizing induced pluripotent stem cells and instead differentiating them into atrial cells has been a promising approach. By mimicking the natural process in the embryo through the use of proteins or small molecules, signaling pathways that cause the specification into certain cells can be activated. This process has to be tailor-made for each cell type as we need to work with the natural programming of a cell to let it become a specific type while suppressing the normal tendency of pluripotent stem cells to differentiated into various cells types.
For heart cells this is done by manipulating the “Wnt” signaling pathway. By activating and deactivating it, pluripotent stem cells are first nudged into becoming mesoderm cells and subsequently cardiomyocytes (heart muscle cells). This has so far been usually applied to produce ventricular cardiomyocytes, but through the addition of retinoic acid atrial muscle cells could also be differentiated already. If you want some more detail check out this link explaining Wnt signalling for heart muscle differentiation, it goes into specifics but it is worth a look to just have an idea of what your cardiomyocytes have been through to get where they are.
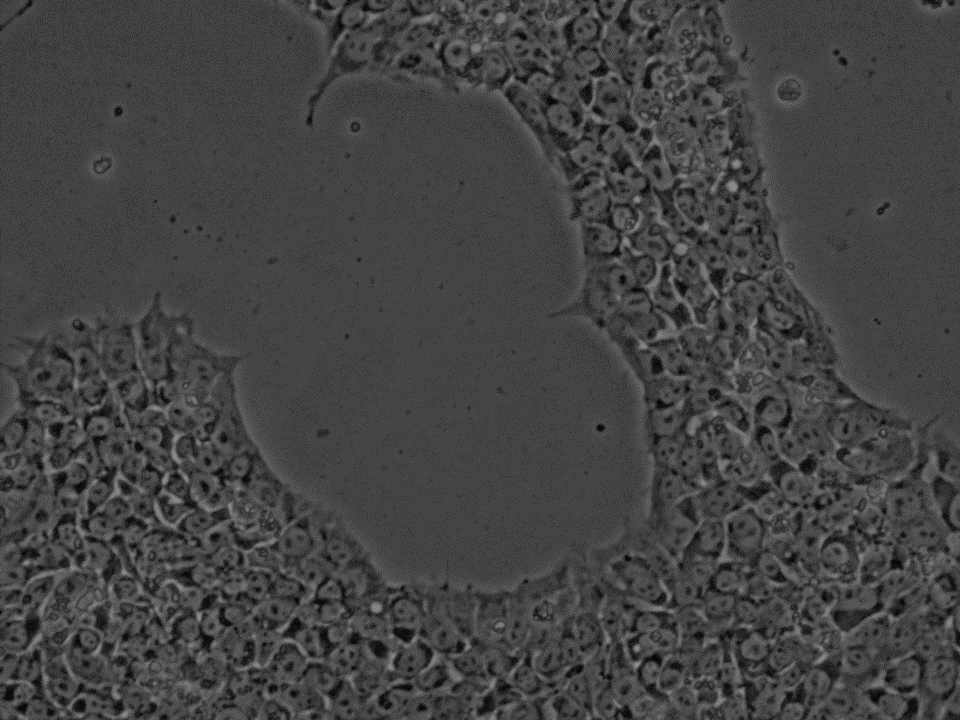
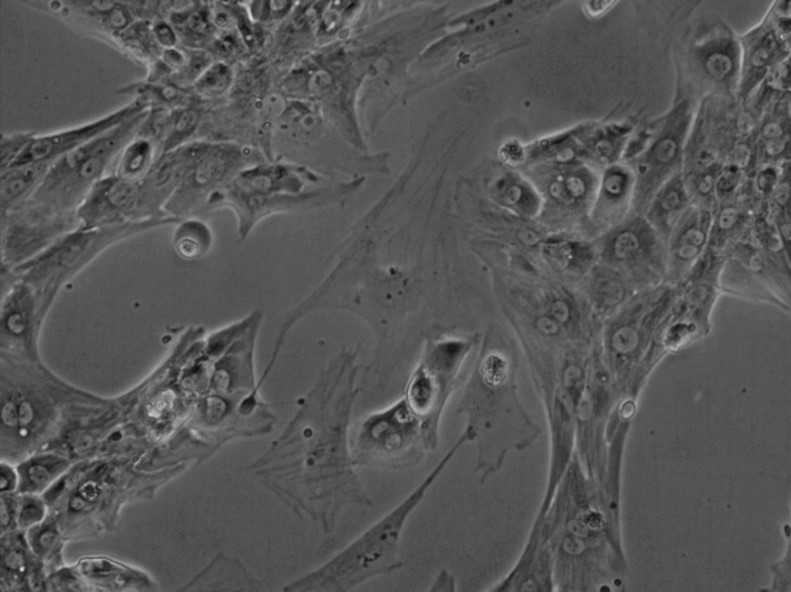
By now you might be inclined to call this an open and shut case, you have some cells, give them some factors and you are done, – early weekend. But for one our body has whole libraries of differing genes and factors which interlock into mind boggling signalling network on which scientists diligently research to find which string to pull to end up with a specific cell like atrial cardiomyocytes. And sometimes even knowing if you ended up with atria cells might be just as hard. While human induced pluripotent stem cells differentiate into cardiomyocytes they can show characteristics of all types of cardiomyocytes, making specification not a distinct but a continuous process of characterization. As you remember atrial cells should beat faster, have shorter action potentials, and some specific ion channels in comparison to ventricular cells. Let’s say only two of these are represented in a cell population, would you call them already atrial? Much like are pancakes breakfast or dinner? – you could get different answers in the US or the Netherlands.
So whats left to do is to work on protocols and factors to nudge the cells just a bit more into the right direction towards the desired characteristics and let the atrial cell type win out the duel of fates.
If I got you interested in knowing more about atrial cardiomyocytes, check out the official Twitter and LinkedIn PersonalizeAF, as well as the hashtag #PersonalizeAF, to learn more about atrial fibrillation and how research is done towards curing it.
See you next time, I have to get back to figuring out if pancakes are dinner.
Thomas Hutschalik
