This past month I took it easier with experiments as we had a three-week workshop, which in normal condition would have seen all personalizeAF ESRs gathered in Valencia. As you may guess, none of us had the chance to travel there. Nevertheless, I have to say that we were pretty good at networking virtually!
Anyways, November had pauci experiments sed moni, and mostly exciting! This time, not with cells but directly at the tissue level (which was already pretty cool and enough for me to be enthusiastic). I’ll keep it simple – I took some atrial tissue, attached its extremities to two springs linked with motion sensors, and applied a preload while stimulating it electrically.
Before proceeding with describing the experiment, let me try and explain some terminology. Preload is defined as the amount of stretch that the tissue (thus, the myocytes) experiences at the end of diastole (prior contraction). Ideally, during experiments preload application is highly suggestable, because it allows tissue or cells to experience an environment which more closely resembles native conditions. The afterload is the pressure that the heart has to overcome to eject the blood during systole (during contraction). The inotropic state is associated with myocardial contractility; depending on whether the muscle is able or unable to move a heavier blood load faster than what is possible with normal myocardium at a given preload, it is referred to as positive or negative, respectively. As stated by the Frank-Starling law, the highest the applied stretch (preload), the highest the force generated upon contraction and therefore the ejected blood volume (stroke volume). Increasing the preload, increases calcium sensitivity of the myofilaments, thus the active tension developed by muscle fibers and the velocity of fiber shortening at a given afterload and inotropic state.
So here we are with tissue under highly controlled mechanical environment. Atria are not functionally required to produce as much force and in normal condition their peak of contraction has lower amplitude compared to ventricles. However, to better understand the difference between atrial and ventricular contractile behavior, it is possible to increase force generation via drug stimulation.
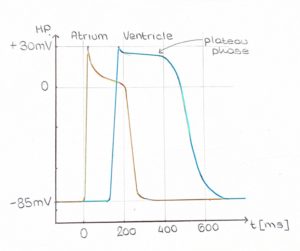
From the electrophysiological perspective, atria are characterized by a shorter action potential (AP), with a non-so-flat plateau phase (Figure 1). As you may already now, heart contraction is initiated by electrical stimuli, therefore it is not surprising that this difference in AP shape results in a different contraction waveform. Due to their different electrophysiological properties, atrial tissue has a steeper and almost instantaneous peak (Figure 2, yellow trace), whereas ventricular tissue has clearly distinguishable contraction and relaxation slopes (green trace).

Next step today is inducing atrial fibrillation, wish me luck!
Teresa
